Personalised medicine: A window into the future
As DNA research continues, scientists are making significant progress on the road to perfecting personalised healthcare
A series of robotic arms move in tandem collecting minute samples of fluid from a set of multicoloured test-tubes. The fluid is deposited in another set of glass vials that automatically start to vibrate, creating whirlpools inside the small jars. Scientists wearing blue rubber gloves and oversized plastic goggles observe the process, their eyes fixed on a large plasma screen showing rows and rows of coloured spots. In every corner of the lab sophisticated machines buzz and whir, each occupied with an infinitely precise task that cannot be trusted to the human hand: mixing, measuring, extracting and decoding. In the far corner another machine engraves aluminium plates with rows and rows of little circles, each one nanometre in diameter, each containing a minute portion of the human genome, ready to be read by a super computer. Just one of those little metal plates costs thousands of dollars, and could just hold the key to the future of medicine.
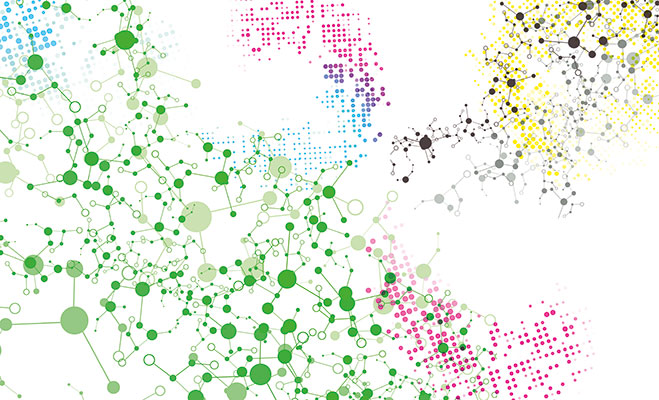
However, this room is not a set in a science fiction film, it is one of many such laboratories all over the world that decodes an individual’s DNA and maps out their genetic material. This is the first step toward what experts are calling ‘personalised medicine’, “a medical philosophy that uses a person’s individual clinical, genetic, genomic, and environmental information to tailor a treatment plan that will maximise efficacy and safety for that individual,” according to Paul Wolpe, Professor of Bioethics at Emory University.
Today scientists are able to genotype not only human DNA but also the DNA of specific diseases
Personalised medicine is being hailed as the future of medicine. The idea is that if we know in detail each patient’s individual traits, we can treat them efficiently, safely and cost-effectively. It is based on two developing technologies: genetic-testing and targeted pharmaceuticals. By testing a person’s genetic material, it will be possible to identify particular genetic profiles and genotypes that will influence the likelihood of an individual developing certain diseases, what course these diseases will proceed through, and other factors such as the individual’s metabolic rates, which affect how drugs are absorbed and processed in the body. By analysing a patient’s genetic profile it will be possible to determine how they might react to certain medication, and drug treatment will be far more adequate to each patient’s needs.
Just ten years ago, getting your genome mapped for personalised medicine would have cost over $75,000 in one of a handful of private labs in the US and would have scarcely been available elsewhere in the world. But the industry has moved in leaps and bounds since then. Today for a mere $300 it is possible to get a basic genetic screen that will reveal predisposition to the most common forms of cancer, other genetic diseases like Parkinson’s, Type-2 Diabetes and even chronic joint pain, as well as metabolic rates for drug absorption and genetic traits such as muscle performance. There is no need to go to a lab or visit a geneticist. Collection kits are mailed to and from the lab and a small spittle in a little plastic test tube provides more then enough genetic material for testing. Within two to three weeks the results are made available online, complete with a range of easy-to-read graphs and detailed reports on specific findings. . The most complete testing currently costs around $5,000 and produces an intricately detailed analysis of genetic material and reveals complexities about the body, and how it is likely to change and deteriorate over time. This more expensive genetic service investigates each individual’s drug responses and gene mutations.
The process has been used for a number of years to identify causes of diseases of difficult diagnosis, and was previously too expensive to be commercially viable. Companies that offer this type of genetic mapping are often research facilities as well, working in tandem with pharmaceutical companies, providing the bioinformatics and genetics needed for whole genome studies of human disease or drug response.
The gene game
Genetic testing has been used for a number of years, especially to assist in the diagnosis of genetic conditions such as Huntington’s disease. It has also been available for people who have a family history of certain types of cancer, who can choose to know if they are likely or not to develop the disease. Doctors believe that prediction can lead to an early diagnosis by increasing the frequency of screening for people who are more likely to develop these conditions. Early diagnosis drastically reduces the cost of treatment and improves survival rates. But this type of predisposition testing can also open the door to more drastic responses. Some women have opted to remove their breasts or ovaries when a genetic screening shows they are likely to develop cancer. However, it is unquestionable that personalised medicine will bring countless advances to the medical field. “Despite many advances in the drug therapy for many diseases, treatment remains suboptimal for a significant proportion of individuals because of unpredictable side-effects of medication or lack of response from the patient,” says Wolpe. Anti-depressants for instance, are notorious for their wildly discrepant reactions in different patients; a simple genetic profile would, in theory, be able to determine what types of patients are more suited to what types of medication, and the doses required.
With all this research, pharmaceutical companies now have a better idea of how their drugs work, and why they occasionally fail
The field of genetics has developed at a staggering pace in the past twenty years. Today scientists are able to genotype not only human DNA but also the DNA of specific diseases. Each cancer has its own genetic information; complete with the gene mutations that cause the abnormal growths. By genotyping the disease – in a case-by-case fashion – for the first time ever researchers are getting a glimpse at what is causing its development and how to tackle those faulty mutations without harming other, healthy cells. This process is still in its infancy, but researchers are confident that soon the disease can be conquered. Drugs can now be developed to target specific metabolising agents in the body, treating diseases at their root cause. This type of drug testing is known as pharmacogenetics. Having access to large pools of genetic profiles will almost certainly help streamline drug research and clinical testing. In the long run, personalised medicine will save hospitals, insurance companies and patients lots of money through targeted therapies which will help avoid less successful treatments. Collective genetic profile statistics will also enable national health providers such as the NHS to choose the best overall drug treatments for the population.
With all this new research, pharmaceutical companies now have a much better idea of how their drugs work, and why they occasionally fail. In an attempt to perfect their products, some pharmaceutical companies are partnering up with private labs to develop simple genetic tests to accompany their drugs. The tests determine if the patient is likely to respond well to the medication, and what dose should be administered. That is the case for Warfarin, a blood thinner notoriously difficult to dose. In 2008 the American Food and Drug Administration started recommending patients prescribed the drug to undergo a genetic test in order to determine the appropriate dosage and thus avoid complications and even in some very rare occassions, death. The genetic tests are expensive but “avoiding one hospitalisation could underwrite the cost of the test for 100 patients,” according to Dr Robert S Epstein, chief medical officer at Medco Health Solutions, the pharmaceutical company behind Warfarin.
However, pharmacogenetics is an expensive process. Right now, large pharmaceutical corporations test irrespective of DNA, and so the pool of research is developed somewhat randomly. Standard practice does not involve testing developing drugs on groups with specific genetic profiles. As a result, drug tests are carried out in genetically random cross sections of a population. If there are too many adverse reactions, the drug is scrapped.
This way companies can cast the medication’s net as widely as possible; a ‘blockbuster drug’ that will corner the market for treatment of a specific type of illness and help a vast number of patients. With any luck, the new product will sell well, generate billions of dollars in profit, and pay for its research many times over, enabling pharmaceutical companies to invest in new research for new drugs.
Personalised medicine providers are planning on selling their services to employers, expressly in the US, where healthcare is part of employment packages
But with the arrival of genetic mapping technology, pharmaceutical companies are reassessing their approach to research. Because it is now possible to determine what types of genetic profiles are likely to respond well to any particular treatment, and why sometimes drugs have adverse or no effects at all, medication is becoming increasingly bespoke. The possibility of blockbuster drugs is dwindling. Pharmaceutical companies are being forced to embrace the potential benefits of niche market drugs with high success rates. The trouble is research and development costs are » too high for drugs that will only ever have the potential to be sold to a fraction of the population. The gamble is that increased safety and high success rates will encourage the use of the treatments and make up for the smaller markets for each drug. Pharmacogenetics will also help to salvage drugs that have previously been deemed failures. Sometimes drug development is aborted when too many patients have adverse reactions. Through genetic testing, it will be possible to identify what caused the bad side effects, and who is likely to suffer from them. If the drug is still successful in a portion of the population, it might still be commercially viable, albeit on a smaller scale. Genetic testing will minimise the number of drugs that get completely abandoned, thus helping to make research budgets much more efficient.
From blockbusters to flops
Cystic fibrosis is a chronic disease that affects one in every 2,000 new-borns. Because of a genetic mutation, the lungs of people with the condition are unable to clear away mucous, causing chronic infections and permanent damage to the organs. In later stages lung transplants often become necessary. The disease is nearly always fatal, and most sufferers do not make it past the age of 30. Through genetic testing, a private lab in the US has managed to identify the genetic mutation that leads to the faulty protein. There are over 1,800 variations that cause the disease, but through extensive research the lab managed to produce two drugs that will work on the majority of mutations. The treatment makes cystic fibrosis a manageable disease, not a life sentence. But it comes with a hefty price-tag; just one year of treatment costs $294,000.
There are also the millions of dollars the lab spent on over 10 years of research. That value is slightly offset by less frequent hospital visits and overnight stays for emergency treatment. When put in treatment from a young age, it is less likely that sufferers will require lung transplants, relieving a massive burden on the system. With so many variables, it is still difficult to determine if the drugs will be economically viable, both for the patients and the labs producing them.
When pharmacogenetics are prevalent it is likely pharmaceutical companies will try to develop new drugs for the most common genotypes or genetic profiles that best respond to treatment. It will be more economically viable for companies to develop drugs that effectively treat the greatest variety of genetic profiles and the most dominant.
But by actively favouring the most prevalent genotypes pharmaceutical companies might risk making whole sections of the population ‘therapeutic orphans’; large groups of people with genotypes that will be deemed too difficult to treat, and thus less likely to receive adequate medical care. This is an issue that has started to be addressed though legislation.
The US and EU have both already began extensive grant programmes for research and development on ‘orphan medications’.
Genetic mapping will make available information that is inherently private. Even if names are removed in databases, DNA is unique and always traceable to the source
Personalised medicine is so far only widely available in North America and parts of Europe. However, in the US it has already started to generate a minor avalanche of insurance reimbursement problems. Wolpe describes instances of unequal treatment of two individuals with the same disease diagnosis: “Two persons may have slightly different mutations of the same gene, both predisposing them to a genetic disorder. One’s common genotype requires $500 worth of pharmacogenetic medication per year, the other’s rare genotype requires $100,000. How will the insurance system handle this disparity?”
In many states in the US the law already allows for long-term care, disability and life insurers to discriminate based on genetics. Someone making more expensive claims will always be charged higher premiums, but health and life insurers might start denying coverage for people with predispositions to incurable diseases, or difficult to treat genotypes. In this case, personalised medicine might also become an intolerable financial burden around the neck of everyday citizens.
But in some ways, personalised medicine is opening new avenues of business within the medical industry. Personalised medicine providers are planning on selling their services to employers, particularly in the US, where healthcare is part of the employment package. Companies have so far been receptive, eager to pay higher healthcare fees for improved treatment outcomes and, crucially, lower prescription costs.
Mapping the future
Scientists are already envisioning a future where a genetic map of any type of disease or cancer will point the way to treatment. With accessible genetic testing for a patient seeking treatment, doctors will know exactly what dose of the exact drug someone will require.
Deadly diseases will become more manageable and predispositions for chronic conditions will be offset. But there is still a lack of understanding; the more researchers look into genomes, more and more new complexities arise. Not all conditions relate to a single gene like cystic fibrosis; Type-2 diabetes for instance relates to at least 18 different genes. For research to progress successfully and start to tackle big diseases like diabetes and cancer, scientists are going to have to start studying larger and larger pools of genetic profiles. Any widespread use of personal medicine will undoubtedly rely on a more systematic application of genetic testing.
The fetishisation of genetics is something that needs to be handled very carefully. If too much emphasis is put on genetic profiles as diagnosis tools, we run the risk of downplaying environmental factors. Even a person with a small genetic propensity to heart conditions might develop one if they are excessively overweight and don’t exercise.
And if, sometime in the future, humanity is entirely genotyped, then the door could be left wide open to genetic discrimination, or some form of eugenics. For all the potential benefits of personalised medicine, the field of genetics could also be seen as an ethical minefield which needs to be universally regulated. In countries such as Britain, where health services are nationalised, the strain that personalised medicine will put on the system are incalculable. Without appropriate consideration and regulation, personal medicine might not ever achieve its full potential as a life-saving approach to medicine.
The future of personalised medicine will rely on costly widespread genetic mapping which has the risk of overburdening an already fragile healthcare system. There is also the chance that healthy individuals might not want to have their genomes mapped. There are real issues of privacy involved in this matter. Genetic mapping will make available information that is inherently private. Even if names are removed in databases, DNA is unique to every individual and is always traceable back to its source. Even in the name of science, it isn’t surprising that people might be reluctant to have personal information made public.
James Watson, the legendary scientist who discovered the DNA double helix, was one of the very first people to have his DNA mapped several years ago. Watson, then already an old man, is reported to have agreed to the process with the condition that no one look at the genes associated with Alzheimer’s disease. He said he simply did not want to know.
And it is easy to see why; Alzheimer’s is a brutal degenerative condition, and it is incurable. Like the scientist, not many people would like to receive this type of information. Some scientists would like to see widespread testing of all newborns at birth, but we must ask how this would affect the lives of these children. Born healthy, but with a higher-then-average chance of maybe one day developing a degenerative disease, it would be like a death sentence at birth, and it could be argued as a clear violation of these children’s privacy.
Right now the main obstacle to the development of personalised medicine as a viable and lucrative business model is the high cost of investment. Before we can seriously consider the widespread use of genetic mapping to treat diseases on an individual basis we must first consider how much we do not know, and how much technology still has to be developed before we can fill these gaps.
“Even if you spend a lot of money and get your genome sequenced, you might think you are going to understand a lot but in reality you probably won’t. We only know the genetic basis for 200 or so genes that you can actually do anything about, or even understand. Most of those are incredibly rare. But there is not enough information to know how to interpret our genome information. That might not be true forever, but it is true right now,” says Dr Michael Snyder, Professor of genetics at Stanford University in California. The human genome has billions of genes with an infinite variety of combinations, it will still be years before we understand it all and all its complexities.
There is very little data on how genetic and non-genetic factors interact, and how these interactions might affect treatment. Researchers are not even sure if individuals respond consistently to a drug treatment over a long time. And there is always the chance that the genetic testing required for pharmacogenetics will turn up far more diseases than cures.